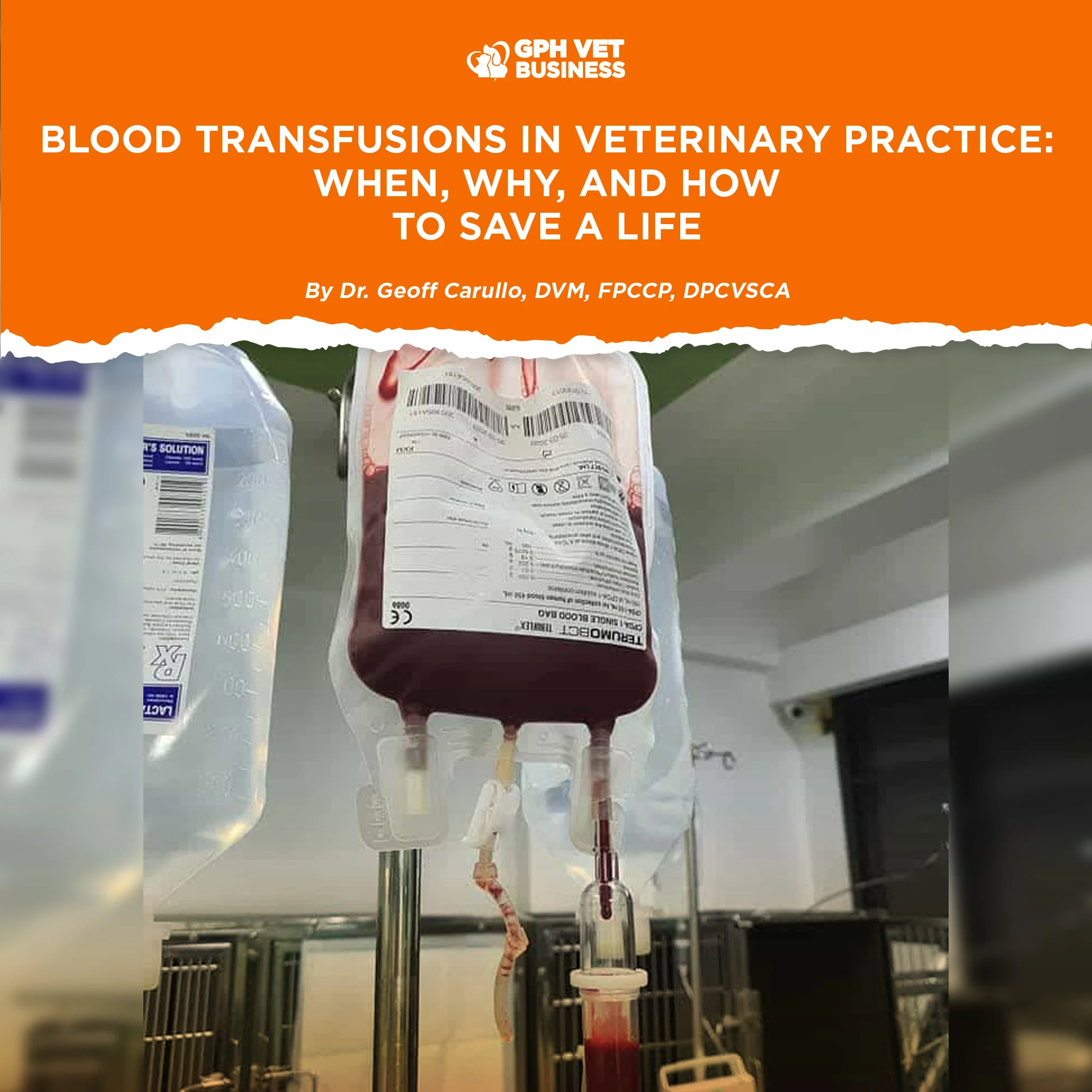
Blood Transfusions in Veterinary Practice: When, Why, and How to Save a Life
By Dr. Geoff Carullo, DVM, FPCCP, DPCVSCA
Blood transfusion is one of the most powerful life-saving tools in veterinary medicine. Yet it remains one of the most delayed interventions in small animal practice. Many patients do not die because blood is unavailable, but because transfusion is initiated too late. Understanding when to transfuse, how much to give, and how to manage complications is essential for every clinician handling emergency and critical cases.
Blood transfusion is not about correcting a laboratory value. It is about restoring oxygen delivery, circulatory stability, and tissue perfusion.
1. Immediate Treatment Priorities in Hemorrhagic Shock
In patients suffering from major hemorrhagic shock, the immediate priorities are:
- Restoration of intravascular volume
- Improvement of cardiac output
- Restoration of blood oxygen content
Crystalloids and colloids may temporarily restore circulation, but only blood products restore oxygen-carrying capacity.
2. Indications for Blood Transfusion
Red blood cell transfusion is indicated whenever the oxygen-carrying capacity of the blood is insufficient to meet metabolic demands. This may result from:
- Acute blood loss
- Chronic blood loss
- Hemolytic anemia
- Decreased red blood cell production
- Refractory shock with poor tissue perfusion
3. Common Causes of Blood Loss Anemia
- Trauma
- Coagulopathies (congenital deficiencies, anticoagulant toxicity, liver disease)
- Platelet disorders (thrombocytopenia, von Willebrand disease)
- Splenic rupture (trauma, torsion, neoplasia)
- Gastrointestinal hemorrhage
- Epistaxis due to infection or neoplasia
4. When Should a Transfusion Be Considered?
There is no absolute “magic PCV.” The decision to transfuse depends on:
- Speed of anemia onset (acute vs chronic)
- Severity of clinical signs
- Cardiovascular and respiratory status
- Response to fluid therapy
- Risk of continued blood loss
However, most clinicians agree that serious impairment of oxygen transport occurs below a PCV of 20%, and many recommend intervention when PCV falls between 20–30%, especially in unstable patients.
5. Clinical Indicators Suggesting the Need for Transfusion
Transfusion should be strongly considered when one or more of the following are present:
- Acute loss of >30% of blood volume (≈30 ml/kg)
- Hematocrit <20%
- Plasma protein <3.5 g/dL
- Ongoing blood loss unresponsive to crystalloids or colloids
Signs of hypovolemic shock:
- Pale mucous membranes
- Prolonged capillary refill time (>2 seconds)
- Tachycardia (>180 bpm)
- Tachypnea (>60 breaths/min)
- Hypotension (MAP <80 mmHg)
- Decreased central venous pressure (<0 cm H₂O)
6. Rate of Blood Administration
Life-threatening hemorrhagic shock:
Administer blood as fast as possible using pressure infusers and large-bore catheters.
Routine replacement therapy:
Recommended rate for whole blood or blood products is 10–22 ml/kg/hour.
The risks of rapid transfusion are outweighed by the risk of death due to hypoxia.
7. Management of Acute Hemorrhage During Surgery
Initial steps include estimating blood loss and deciding whether replacement is required. Many healthy animals can tolerate acute loss of up to 10% of blood volume, and in some cases up to 40–50%. Critically ill patients, however, may not tolerate even minimal losses.
If:
- PCV remains above 20%
- Plasma protein remains above 3.5 g/dL
- Blood pressure is adequate
Blood transfusion may not be necessary. If these parameters deteriorate or the patient becomes unresponsive to conventional therapy, whole blood transfusion is indicated.
8. Autotransfusion
Autotransfusion involves collecting and reinfusing the patient’s own blood, usually from the thoracic or abdominal cavity, during severe acute hemorrhage when blood products are unavailable.
While risks include contamination, coagulopathies, and embolism, autotransfusion can be life-saving in emergency situations.
9. Risks of Blood Transfusion
Potential risks include:
- Acute and delayed hemolytic reactions
- Anaphylaxis
- Transmission of infectious agents
- Citrate toxicity (hypocalcemia)
- Circulatory overload
Despite these risks, transfusions are generally safe when performed correctly.
10. Assuming Whole Blood Transfusion Is Needed: How Much Blood Should I Give?
Once the decision to transfuse has been made, the goal is to raise the hematocrit enough to restore oxygen delivery without causing volume overload.
A. Rule of 1s (Fast and Practical)
- 1 ml of whole blood per pound body weight raises PCV by approximately 1%
- Equivalent to 2.2 ml/kg to raise PCV by 1%
- Example:
A 20-kg dog needing a 5% PCV increase:
20 × 2.2 × 5 = 220 ml of whole blood
B. Standard Clinical Estimates
- 20 ml/kg of whole blood raises PCV by approximately 10%
- 10 ml/kg of packed red blood cells raises PCV by approximately 10%
C. Hemoglobin-Based Formula
When donor hemoglobin concentration is known:
Volume (ml) =
Body weight (kg) × desired Hb increase (g/dL) × 70 ÷ donor Hb (g/dL)
D. PCV-Based Formula (Most Accurate)
When donor PCV is known:
Volume (ml) =
Body weight (kg) × 90 ml/kg × (Desired PCV − Patient PCV) ÷ Donor PCV
The disadvantage of the hemoglobin- and PCV-based formulas is that donor values must be known. In emergencies, practical estimates are often preferred.
11. Transfusion Reactions and Recognition
Acute Hemolytic Reactions
- Fever
- Tachycardia
- Vomiting
- Hypotension
- Collapse or seizures
Action: Stop transfusion immediately and initiate aggressive supportive care.
Delayed Hemolytic Reactions
- Fever
- Icterus
- Anemia days to weeks later – Usually mild and self-limiting.
Non-Hemolytic Hypersensitivity Reactions
- Urticaria
- Pruritus
- Facial swelling
- Respiratory distress
- Mild reactions may resolve by stopping the transfusion alone.
12. Preventing Transfusion Reactions
- Use universal donors when possible
- Cross-match donors and recipients
- Proper storage and handling of blood products
13. Blood Types You Must Know
Dogs
DEA 1.1, 1.2, 3, 4, 5, 6, 7, 8
DEA 1.1-negative dogs are preferred universal donors.
Cats
Blood types: A, B, AB
Type A is most common. Cross-matching is critical due to naturally occurring antibodies.
Final Thoughts
Blood transfusion is not a last resort. It is a decisive intervention that restores oxygen delivery, stabilizes shock, and saves lives. Delaying transfusion out of fear often causes more harm than the transfusion itself.
Clinical judgment saves patients. Numbers only guide you.
Sharing this helps others understand what it really means to be a vet. Like and follow if you’re with us.